How Long Can Dakin's Solution Be Used on a Wound
Authors
- Levine, Jeffrey Yard. MD
Abstruse
Abstruse: Dakin's solution has been used for nigh a century. Information technology is a dilute solution of sodium hypochlorite, which is commonly known equally household bleach. When properly applied, it tin can kill pathogenic microorganisms with minimum cytotoxicity. This article reviews its history and discusses how evolving applied science might pave the style for a new function for this antiseptic.
Commodity Content
INTRODUCTION
It tin can be easy to forget that the evolution of wound care is forged in war, human suffering, and the progress of culture.1 In the 20th century, wound care became intertwined not just with history, merely with development of modern science and technology. The story of Dakin'due south solution illustrates non only the intersection of medicine and history, but also demonstrates how medical advances owe their genesis to the struggle and lives of individuals. Dakin'southward solution has been function of the wound intendance armamentarium for near a century, and the men responsible include non only the biochemist Henry Drysdale Dakin, PhD, (Figure i) but likewise Alexis Carrel, MD, an aggressive Nobel Prize winning doc whose science and politics went darkly wrong. Were information technology non for Dr Carrel, the solution created by Dr Dakin would be unknown to the states today.
 | Figure 1. HENRY DRYSDALE DAKIN (1880-1952) |
Dakin's solution is just a dilute mixture of sodium hypochlorite-the principal ingredient of household bleach. Sodium hypochlorite is used to whiten dress, remove stains, and to disinfect kitchens, bathrooms, and swimming pools. Undiluted household bleach comes every bit a v% solution of sodium hypochlorite, and "full-forcefulness" Dakin'due south is sold over-the-counter as 0.five%, or 1/100 of the household concentration. This is the concentration recommended by the Centers for Disease Control and Prevention (CDC) equally an constructive disinfectant.2
In its concentrated grade, sodium hypochlorite can liberate dangerous amounts of chlorine or chloramine if mixed with acids or ammonia, and anhydrous sodium hypochlorite is explosive.iii Ingestion can cause vomiting and corrosive injury to the gastrointestinal tract, and skin contact causes chemical burns and liquefactive necrosis. When properly diluted and applied, a buffered solution of sodium hypochlorite tin can kill pathogenic microorganisms with minimum cytotoxicity. This article reviews the history of Dakin's solution and discusses how evolving wound intendance technology might create an expanded role for this time-honored antiseptic.
HENRY DAKIN AND ALEXIS CARREL ARRIVE IN NEW YORK CITY
Henry Drysdale Dakin, PhD, was built-in in London in 1880 and studied at the Lister Institute of Preventive Medicine.4 He was interested in biochemistry and performed studies on enzymes and amino acid metabolism when the field was in its infancy. He came to the United States in 1905 on the invitation of Christian Herter, MD, a wealthy New York Metropolis physician affiliated with Bellevue Hospital Medical College, who established a research laboratory on the tiptop flooring of his home on Madison Artery. In the Herter Laboratory, Dakin experimented with the chemistry of proteins, working alone and unknown until developments in world history conspired to make his name part of the wound care dictionary.
Alexis Carrel, Md, was built-in in a hamlet nearly Lyon, French republic, in 1873. His mother was an embroiderer, which may have set the phase for his involvement in suturing.5 He studied medicine at the University of Lyon and specialized in surgery. His perfection of techniques for anastomosis of blood vessels in 1902 at age 29 would revolutionize vascular surgery and make organ transplantation possible. He came to N America in 1904 and spent time in Montreal, Quebec, Canada, then continued on to the University of Chicago where he connected his experiments on anastomosis of blood vessels and organ transplantation.
Dr Carrel built a reputation that gained the attention of Simon Flexner, director of the Rockefeller Constitute of Medical Research in New York Urban center, New York, where Carrel began work in 1906. He experimented with surgery of the heart, blood vessels, and organ transplantation, and, in 1912, he won the Nobel Prize for physiology and medicine in recognition of his studies in vascular anastomosis.6 Carrel had the stardom of being the youngest Nobel laureate and the get-go American scientist to win the Prize.
Both Drs Dakin and Carrel were in New York Urban center at the bidding of wealthy patrons who wished to accelerate medicine. The Herter Laboratory where Dr Dakin worked was on Madison Artery near 68th Street, and the Rockefeller Plant was six blocks east on York Artery and 66th Street. In the rarefied world of science and society, it is probable that the Nobel Prize winner and Dr Dakin knew of each other's work.
THE COLLABORATION OF DAKIN AND CARREL IN WORLD WAR I
On June 28, 1914, Archduke Franz Ferdinand of Austria was assassinated, triggering the onset of Globe War I. On August 1, 1914, Federal republic of germany declared war on France, and soon later, Dr Carrel returned to his native homeland to run a war machine infirmary and research center funded by the Rockefeller Foundation. Dr Dakin accompanied Carrel to the war zone, where he would direct the chemical laboratory and reach the piece of work that would make his name part of wound intendance history.
By 1915, the Western Front was marked by the deadly tactic of trench warfare. Vast areas of interwoven trenches and dingy dugouts became killing fields for hundreds of thousands of soldiers on both sides. History tells us that the greatest killer was not bullets or shrapnel, merely disease and infection. Wounds in trench warfare combined tissue damage with deeply embedded droppings, including mud and human waste.7 Clearly, improvements in medical intendance and asepsis would be a tool to win the state of war and foreclose suffering, and this is where the collaboration of Drs Dakin and Carrel created innovation.
Not far from the frontlines, Dr Carrel revolutionized war surgery by pioneering techniques of debridement, cleanliness, and antiseptic methods. In the introduction to his classic work, Treatment of Infected Wounds, Dr Carrel wrote: "The suppression of wound infection would protect a large number of men from incapacity or death, and would bring nearly the rapid restoration to health of the greater number of those whose anatomic lesions are compatible with life. Such progress would result in peachy saving in money and men."8
Dr Carrel reviewed gimmicky medical practices and observed that many surgeons did non use aseptic technique, and inquiry studies of wounds rarely used measurement of bacteria and healing rates. In addition, in that location were few studies that showed quantitative changes in pathogenic bacteria when clarified agents were used. Dr Carrel proposed using a substance that did not irritate skin, even so had sufficient bactericidal power to kill microbes present in a wound. This is where Dr Dakin's work became an essential component of Dr Carrel's innovations.
Dr Dakin developed the antiseptic solution that became the cornerstone of Carrel's surgical method. Dr Dakin tested more than 200 substances, measuring their action on tissues and bacteria before finally deciding on chloramines that tin can exist converted to hypochlorite of soda.ix His goal was to place a solution with minimal tissue toxicity that could sterilize a wound. Dr Dakin meticulously demonstrated his results with quantitative measurement of germicidal action.
The complexity and scope of choosing an clarified is reflected in Dakin'due south book, A Handbook of Antiseptics, which he coauthored with a professor of pathology at Bellevue Hospital.10 The authors review all known chemical antiseptics, their chemical structure, and pros and cons of each. They found that hypochlorites fit the criteria to minimize irritant qualities, while nonetheless maintaining antiseptic action. They observed that the germicidal properties of hypochlorites were brusque acting and ended that the solution should be continuously instilled into wounds.
Using the solution developed by Dr Dakin, Dr Carrel adult techniques to quantify healing. These included measuring the wound surface with traced drawings and planimetry and computing wound volume by measuring h2o poured into the wound. With these methods, Dr Carrel concluded that continuous instillation of Dakin's solution both sterilized wounds and accelerated healing.
Dr Dakin was non listed as coauthor of Carrel's book, titled The Handling of Infected Wounds, but Carrel borrowed extensively from Dr Dakin's writings. A close read of Carrel's volume reveals a nearly complete word-for-word reprint of Dakin's newspaper titled, "On the Use of Sure Antiseptic Substances in the Handling of Infected Wounds."9 Dr Carrel also borrowed liberally from another of the biochemist's publications, which recounted the history and background of the clarified'southward ingredients.eleven It must have been difficult for a biochemist to challenge authorship past a Nobel Prize-winning surgeon and director of a military infirmary in the midst of a world war.
Dr Carrel's surgical technique for wound healing relied heavily on Dakin's solution equally an antiseptic. He preceded its awarding by meticulously removing shreds of article of clothing, projectiles, splinters, blood clots, and necrosed tissue and accomplished careful hemostasis. He warned against packing a contaminated wound as this can protect microbes against antiseptics. Dr Carrel advised practitioners to cleanse and debride the wound every bit soon every bit possible and to localize residual projectiles and foreign bodies using radiography. He devised techniques for continuous delivery of Dakin'due south solution using irrigation through a network of bottles, glass cylinders and stopcocks, and rows of perforated rubber tubes surrounded by absorbent fabrics (Figures 2 and 3). Large syringes with safety bulbs were too used. These techniques were reported by contemporary nurses as messy and labor intensive, merely effective in healing wounds.12
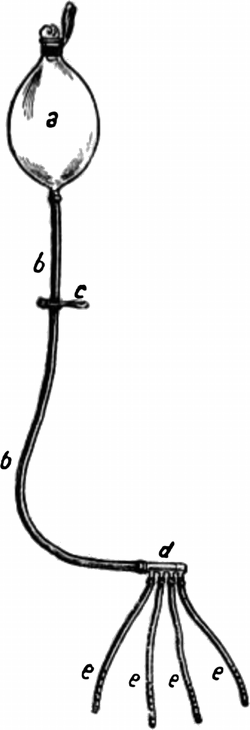 | Figure two. CARREL'S Appliance FOR WOUND IRRIGATION USING THE Clarified SOLUTION DEVELOPED BY DAKIN |
 | Figure 3. NURSE APPLYING THE CARREL-DAKIN WOUND IRRIGATION Procedure |
Dr Carrel demonstrated efficacy of his techniques with clinical observations and quantitative bacterial examination. He measured outcomes, including time for wound closure, subtract in amputations, and diminution in length of treatment. He too provided a cost analysis that showed how decreased inability from utilize of his techniques would result in pension savings paid by the state.13 Dr Carrel made the groundbreaking claim, "[horizontal ellipsis]it has been possible to forestall, in the greater number of cases, infection of wounds and to abolish, almost entirely, suppuration in hospitals."14
DAKIN AND CARREL PART Means BUT THEIR NAMES REMAIN LINKED
Dr Dakin settled with his married woman on an manor overlooking the Hudson River 30 miles due north of New York City. He married the widow of Dr Christian Herter, the patron who brought him to Manhattan and underwrote his experiments with protein chemistry. He continued his research, working alone and living a quiet life every bit his eponymous antiseptic was adjusted past doctors worldwide. The antiseptic, however, bore not only the proper noun of Henry Dakin, but was hyphenated with the name of Alexis Carrel. Review of the medical literature between the World Wars shows many studies referencing the Carrel-Dakin technique and Carrel-Dakin solution.fifteen,16
In contrast with Dr Dakin, who retreated to a secluded country lifestyle, Dr Carrel not only continued his scientific piece of work just too expanded his association with famous and influential people. He returned to the Rockefeller Institute in 1919 and became friends with Thomas Edison and Henry Ford.17 He continued to pioneer new frontiers, developing techniques of tissue culture.18 At the Rockefeller Institute, Dr Carrel became the start to cultivate tumor tissue in vitro-a huge accomplishment in the pre-antibiotic era. In the 1930's, he teamed upwardly with Charles Lindbergh to create a perfusion apparatus designed to keep organs alive outside the trunk.19
Alexis Carrel likewise turned his mind and career toward improving the man race through eugenics-an endeavor that would atomic number 82 him to serve the wrong side of politics and blot his reputation in history. While at the Rockefeller Foundation, he used his research facilities to brood a superior race of mice.19 He summarized his eugenic theories in a book entitled, Man the Unknown. Published in 1935, this best-selling book advocated creation of a human utopia nether the direction of an intellectual aristocracy-a view that echoed the politics of fascism at a time when Hitler and Mussolini were gaining power in Europe.
In blunt and spooky terms, Dr Carrel described his philosophy and programme for "[horizontal ellipsis]the salvation of the white races in their staggering accelerate toward civilization."20 He proposed techniques to mold the human race into a strong and superior grouping using psychology, nutrition, education, and spiritual enrichment. For undesirable people of social club, such as criminals and the insane, Dr Carrel suggested that they "[horizontal ellipsis]should be humanely and economically disposed of in small euthanistic institutions supplied with proper gases."21 When his volume was introduced to Federal republic of germany in 1936, Carrel added praise to the Nazi regime for their "energetic measures" to promote eugenic theories.
During Globe War Ii, Dr Carrel rejoined the state of war effort in Europe. He took a job underwritten past the Vichy regime in occupied French republic, becoming head of an institute named The French Foundation for the Study of Man Problems. Its aim was to investigate the reconstruction of man in the spirit of his book, "Homo the Unknown."22,23 After the Allies reached Paris in August of 1944, Dr Carrel was arrested and defendant of being a Nazi collaborator. He died shortly thereafter on November 5, 1944, at the historic period of 71.24
After the war, the name of Alexis Carrel was dropped from Henry Dakin's clarified solution, but its application for infected wounds continued.
DAKIN'Southward SOLUTION TODAY
The human carnage of World State of war II stimulated a new search for agents that could fight infection. Past 1943, clinical trials had demonstrated penicillin's efficacy as an antibacterial agent, and production was scaled upwards to treat Allied soldiers. The antibody era rendered obsolete the circuitous and labor-intensive irrigation techniques pioneered past Dr Carrel.
In the ensuing years, many other topical antiseptic therapies were developed including bacitracin, chlorhexidine, benzalkonium chloride, iodine-containing agents, and others.25-28 Systemic antibiotics and advances in life support enabled the growth of new medical fields, such as burn science and plastic surgery.29 Past the end of the 20th century, as irresolute population demographics brought an increased prevalence of pressure ulcers and diabetic wounds, other specialties became involved with wound care, including hyperbaric oxygen therapy, podiatry, and vascular surgery.
Henry Drysdale Dakin died on Feb 10, 1952, at the age of 72. His solution continues to be used by today'southward wound care practitioners, but few are aware of its history. In addition, at that place is trivial noesis of the requirement for continuous instillation due to brusk-interim bactericidal properties determined by Drs Dakin and Carrel. And, few contemporary guidelines for its use are available.
In general, topical antiseptics such as Dakin's solution, povidone iodine, and hydrogen peroxide are frowned upon considering of their adverse effects on healthy tissue.thirty Yet, at that place is literature that suggests they can be safely used in certain highly contaminated wounds and that their utilize is cost-effective.31,32 Clinicians know that Dakin's solution is cheap, and it is effective against a broad spectrum of aerobic and anaerobic organisms as well as fungi, including antibody-resistant organisms.33 Dakin'south solution is bachelor commercially at total forcefulness (0.v%), half strength (0.25%), quarter strength (0.125%), and 1/twoscore force (0.0125%). The term "full forcefulness" refers to the highest concentration tolerable to the pare, and the mixture recommended by the CDC as a household disinfectant.2 The production data for all four of these strengths is identical: one time daily for lightly to moderately exudative wounds, and twice daily for heavily exudative wounds or highly contaminated wounds.34 In a literature review performed by Century Pharmaceuticals, they noted no consensus for the utilise of topical antiseptics, and farther research concluded that clinical trials are needed for the best concentrations of Dakin's solution.35
There are many unanswered questions regarding Dakin's solution. In an era of avant-garde wound intendance when so many products are available, what is the best clinical situation for application of this mixture, and for what duration and concentration? Henry Dakin determined that because of its short half-life, the solution must exist applied as a continuous irrigation, so why is information technology recommended only once or twice per solar day?
In a modernistic technological innovation that echoes the techniques developed past Carrel and Dakin, negative-force per unit area wound therapy (NPWT) at present is bachelor with automated irrigation for wound cleansing and removal of infectious materials.36 Topical solutions are cyclically fed into the foam dressing via an boosted set of tubes under negative pressure. Raad et al37 tested NPWT with Dakin's solution irrigation on five patients with venous stasis ulcers with favorable results. KCI lists quarter-strength Dakin'southward (0.125%) as 1 of the solutions compatible with their instillation technology, along with isotonic saline, silver nitrate 0.5%, sulfonamides, and others.38 In a pilot report of NPWT with instillation, Gabriel et al39 describe clearance of infection, earlier wound closure, and earlier infirmary discharge-claims similar to those published past Alexis Carrel in 1917.
There is recent controversy as to whether medical eponyms should be abandoned.40 In the author'due south opinion, eponyms honor history and remind us of our humanity. In the case of Dakin'due south solution, this eponym teaches us that wound care is forged in war and the struggle for the advocacy of medical scientific discipline and civilisation. The antiseptic solution described by Henry Drysdale Dakin has been with the states for decades, and as technology seeks to evolve and button forrad, this apprehensive biochemist teaches that clinicians are not much farther along than they were almost a century ago.
REFERENCES
1. Majno Thou. The Healing Hand: Man and Wound in the Aboriginal World. Cambridge, MA: Harvard University Press; 1975. [Context Link]
2. Centers for Disease Control. http://www.cdc.gov/meningitis/lab-manual/chpt04-biosafety.html. Final accessed May 22, 2013. [Context Link]
three. Agency for Toxic Substances & Affliction Registry. http://world wide web.atsdr.cdc.gov/mmg/mmg.asp?id=927&tid=192. Last accessed May 22, 2013. [Context Link]
four. Obituary: Henry Drysdale Dakin. Lancet 1952; 1 (6704): 426. [Context Link]
5. Whonamedit? A Dictionary of Medical Eponyms. Alexis Carrel. http://world wide web.whonamedit.com/doctor.cfm/445.html. Last accessed May 23, 2013. [Context Link]
6. The Nobel Prize in Physiology or Medicine 1912. http://www.nobelprize.org/nobel_prizes/medicine/laureates/1912/. Last accessed May 23, 2013. [Context Link]
7. Haller JS Jr. Treatment of infected wounds during the great state of war, 1914 to 1918. South Med J 1992; 85: 303-xv. [Context Link]
8. Carrel A, Dehelly Thou. The Treatment of Infected Wounds. New York, NY: Hoeber; 1917: 2. [Context Link]
nine. Dakin HD. On the use of certain antiseptic substances in the treatment of infected wounds. Br Med J 1915; 2 (2852): 318-20. [Context Link]
x. Dakin Hard disk, Kunham EK. A Handbook of Antiseptics. New York, NY: Macmillan; 1918. [Context Link]
11. Dakin Hd. The clarified action of hypochlorites: the ancient history of the "new clarified." BMJ 1915; 2 (2866): 809-10. [Context Link]
12. Male monarch K. Our historical roots: Dr. Richard Drysdale Dakin, DSc, and his solution. J Wound Ostomy Continence Nurs 2008; 35 (3): 289-92. [Context Link]
xiii. Carrel A, Dehelly Thousand. The Treatment of Infected Wounds. New York, NY: Hoeber; 1917: 217. [Context Link]
14. Carrel A, Dehelly Thousand. The Treatment of Infected Wounds. New York, NY: Hoeber; 1917: 8. [Context Link]
15. Ransford-Gay SC. The Carrel-Dakins solution pharmaceutically and physiologically considered. J Am Pharm Assoc 1917; 358: 84-8. [Context Link]
xvi. Cleary EW. The Carrel-Dakin treatment of infected wounds. Cal West Med 1927; 27: 389. [Context Link]
17. Newton JD. Uncommon Friends: Life With Thomas Edison, Henry Ford, Harvey Firestone, Alexis Carrel, and Charles Lindbergh. San Diego, CA: Harcourt; 1989. [Context Link]
18. Carrel A. A method for the physiological study of tissues in vitro. J Exp Med 1923; 38: 407-eighteen. [Context Link]
19. Friedman DM. The Immortalists: Charles Lindbergh, Dr. Alexis Carrel, and Their Daring Quest to Live Forever. New York, NY: Harper Collins; 2007. [Context Link]
twenty. Carrel A. Man, the Unknown. New York, NY: Harper & Brothers; 1935: 291. [Context Link]
21. Carrel A. Man, the Unknown. New York, NY: Harper & Brothers; 1935: 319. [Context Link]
22. Carrel Foundation Maps Study of Human being. New York Times. December 7, 1941. [Context Link]
23. Vichy Endows Piece of work of Dr. Alexis Carrel. New York Times. February ii, 1942. [Context Link]
24. Dr. Carrel Arrested as Vichy Adherent. New York Times. Baronial 31, 1944. [Context Link]
25. Meleney FL, Johnson B. Bacitracin therapy; the start hundred cases of surgical infections treated locally with the antibody. J Am Med Assoc 1947; 133: 675-eighty. [Context Link]
26. Grant JC, Findlay JC. Local treatment of burns and scalds using chlorhexidine. Lancet 1957; 272 (6974): 862-86. [Context Link]
27. Lairtus K. Use of benzalkonium chloride in wound irrigation [in Castilian]. Medicina (Mex) 1957; 37 (770): 190-one. [Context Link]
28. Connell JM, Rousselot LM. Povidone-iodine: extensive surgical evaluation of a new antiseptic agent. Am J Surg 1964; 108: 849-55. [Context Link]
29. Lowbury EJ. Advances in the control of infection in burns. Br J Plast Surg 1967; 20: 211-vii. [Context Link]
30. Bergstrom North, Bennett MA, Carlson CE, et al. Treatment of Pressure Ulcers. Clinical Do Guideline, No. 15. AHCPR Publication No. 95-0652. Rockville, MD: Agency for Health Intendance Policy and Research; 1994. [Context Link]
31. Doughty D. A rational approach to the use of topical antiseptics. J Wound Ostomy Continence Nurs 1994; 21: 224-31.
32. Altunoluk B, Resim Southward, Efe E, et al. Fournier's gangrene: conventional dressings versus dressings with Dakin's solution [published online]. ISRN Urol; 2012. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3329652/. Final accessed May 23, 2013. [Context Link]
33. Cornwell P, Arnold-Long Chiliad, Barss SB, Varnado MF. The use of Dakin'south solution in chronic wounds. J Wound Ostomy Continence Nurs 2010; 37: 94-104. [Context Link]
34. Century Pharmaceuticals, Inc. http://www.dakins.net/products.html. Last accessed May 23, 2013. [Context Link]
35. Century Pharmaceuticals, Inc. http://www.dakins.internet/inquiry/litreview.pdf. Last accessed May 23, 2013. [Context Link]
36. KCI website. http://www.kci1.com/KCI1/vacinstilltherapyunit. Last accessed May 23, 2013. [Context Link]
37. Raad R, Lantis JC 2nd, Tyrie Fifty, Gendics C, Todd M. Vacuum-assisted closure instill every bit a method of sterilizing massive venous stasis wounds prior to split thickness skin graft placement. Int Wound J 2010; seven (two): 81-5. [Context Link]
38. VAC Ulta Negative Pressure Wound Therapy Arrangement Monograph. KCI Licensing, Inc; 2012. [Context Link]
39. Gabriel A, Shores J, Heinrich C, et al. Negative pressure wound therapy with instillation: a pilot study describing a new method for treating infected wounds. Int Wound J 2008; 5: 399-413. [Context Link]
forty. Whitworth JA. Should eponyms be abased? No. BMJ 2007; 335 (7617): 425. [Context Link]
Source: https://www.nursingcenter.com/journalarticle?Article_ID=1585988&Journal_ID=54015&Issue_ID=1585854
0 Response to "How Long Can Dakin's Solution Be Used on a Wound"
Postar um comentário